Editorially Independent Content
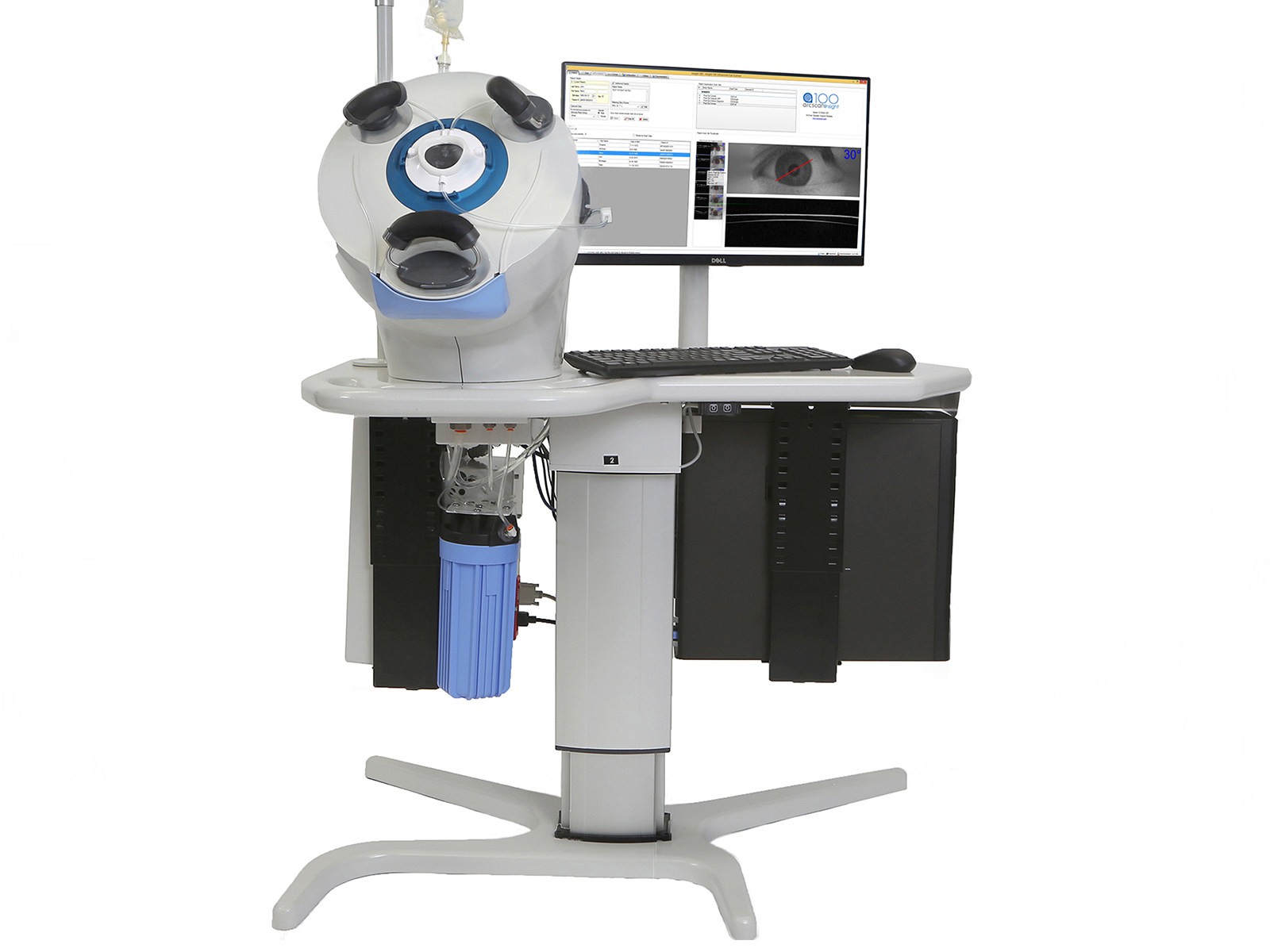
High-frequency ultrasound provides an extremely high level of detail of ocular structures. Not only does it enable visualization behind the iris, the backscatter shows physical discontinuities in the cornea, such as a flap interface 10 years after LASIK. Ever since my residency and fellowship training, I have had a special interest in ultrasound imaging of the cornea. After acquiring countless scans of eyes with photorefractive keratectomy and central islands, early LASIK complications, late LASIK complications, and ectasia, I recognized that patterns began to develop. Combining this information with tomography and topography helped create a better understanding of the cornea and how to prevent and manage corneal issues. The amazing thing is that it has taken 20 years for high-frequency ultrasound to come to market in the form of the Insight100 (ArcScan Inc), a digital, very high-frequency ultrasound-scanning device.
ArcScan refers to this device as being "ultrasound evolved" as it has none of the disadvantages of handheld ultrasound biomicroscopy (UBM). It is more similar to optical coherence tomography (OCT) from both the patient and operator standpoint because there is no direct contact with the eye and measurement is optimized by head stabilization, eye fixation, auto-focusing and precision steering of the ultrasound beam. Therefore, this device can provide the same kind of measurement performance that we are accustomed to from OCT, but also open a broader range of capabilities by using ultrasound instead of light as an energy source.
Zeroing in on Keratoconus
I have had access to the technology for research purposes and use it daily to screen patients for keratoconus or diagnose referral patients with complex pathologies. It is understood that the corneal epithelium changes if you change the shape of the cornea and that keratoconic corneas are different from normal corneas.
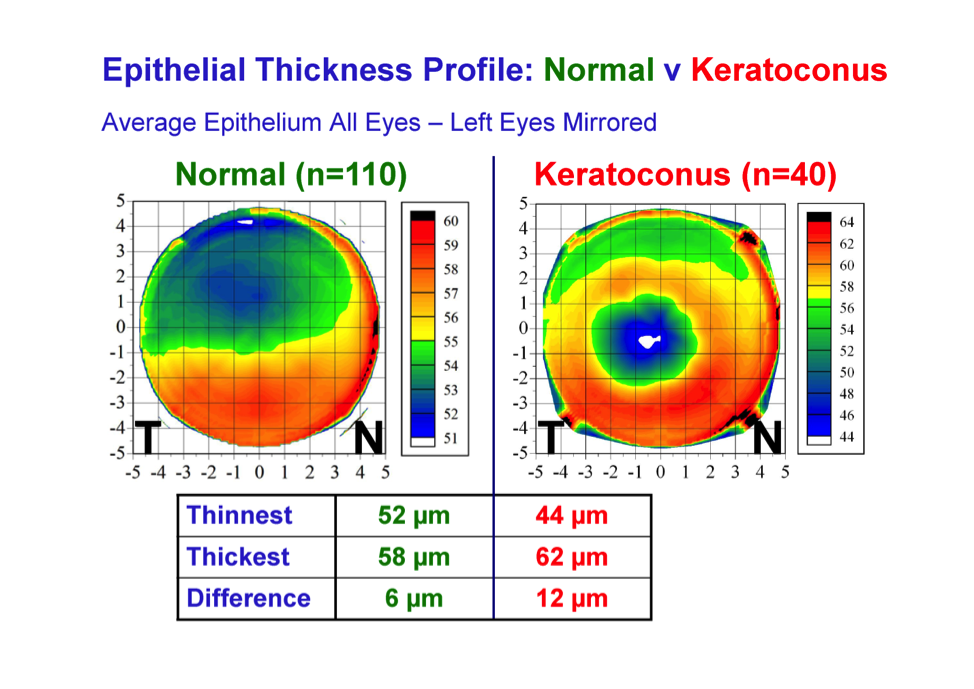
Some refractive surgeons are now convinced that screening for keratoconus with tomography alone does not detect early keratoconus because the extrusion is not sufficient enough to show in the algorithm. For the same price as a typical eye-scanning device, the Insight100 provides a new stream of information.
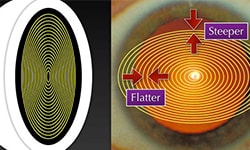
The beautiful thing about combining the latest tomography algorithms with an epithelial thickness map is that the high frequency ultrasound epithelial maps can show as little as 1 or 2 microns of focal thinning in the whole of the 10-millimeter zone. Focal thinning associated with any back surface change is diagnostic of keratoconus.
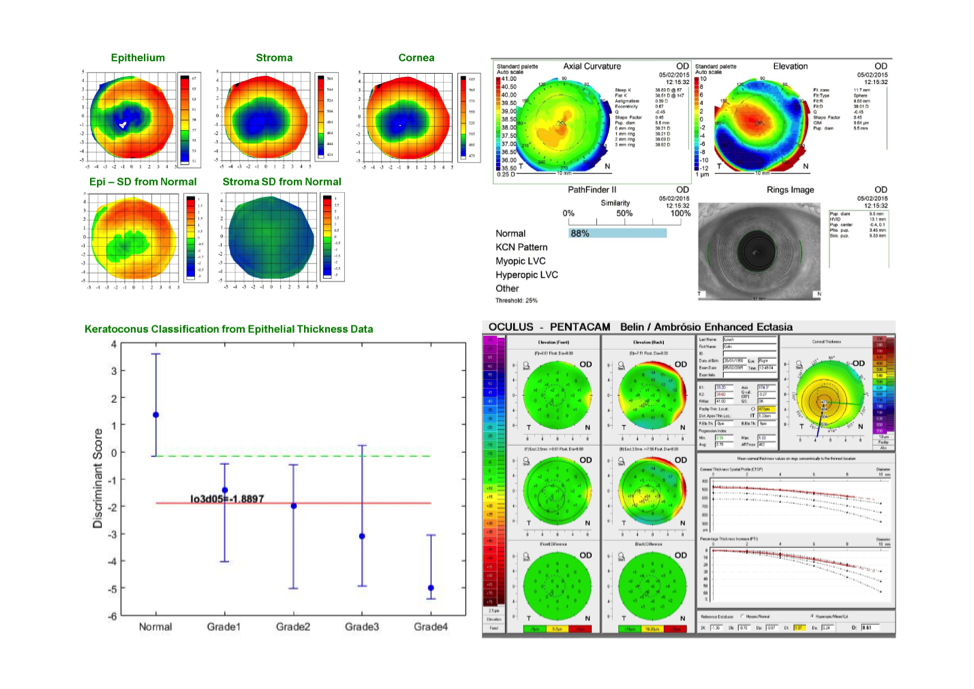
The number of eyes that I examine with totally normal topography and tomography that present with keratoconus based on epithelial thickness screening is not many, but I know to avoid corneal-based refractive surgery on these patients. Furthermore, you can also rule out keratoconus with total confidence in corneas with abnormal topography if the epithelium is thicker over the region of steepening.
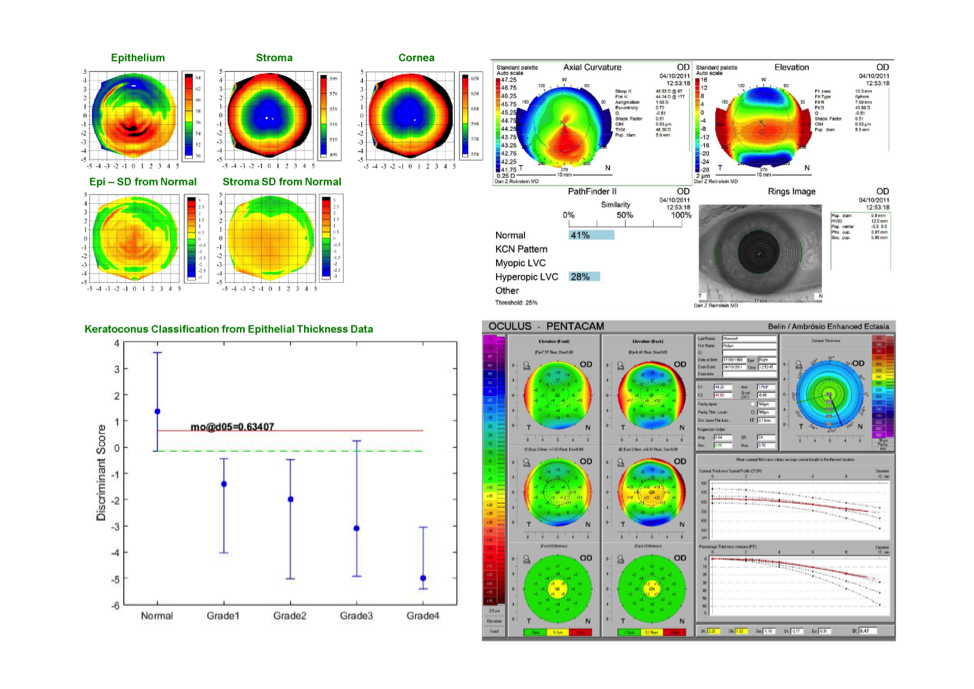
A 1,500-eye screening study finds slightly over 9% of eyes were keratoconus suspect. After looking at the epithelial thickness maps from this group, 14% of eyes were determined to be keratoconic but 86% of them were not. Surgery was performed in those eyes with stable results years later. We have seen a 7% increase in LASIK surgical volume over the past 10 years because the epithelial profiles allow us to rule out keratoconus.
Precise Measurements for ICL Sizing
The other big application for the Insight100 is sizing implantable collamer lenses (ICLs). The ICL is a phenomenal technology and very safe if it is correctly sized.
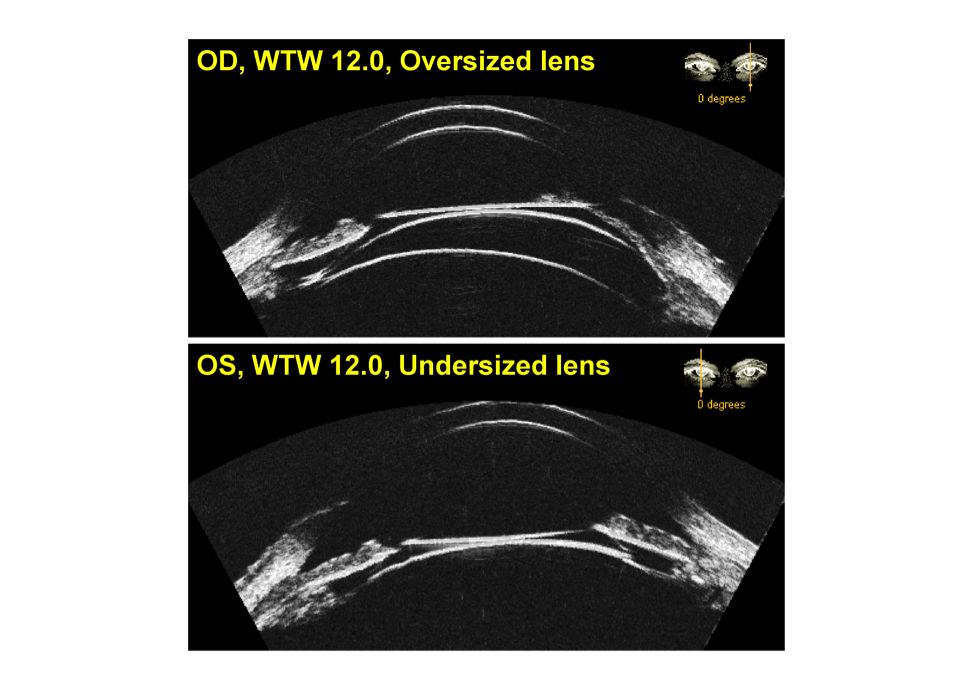
Typically, lens selection is estimated from external ocular measurements of the white-to-white or angle-to-angle. Many studies have been performed to find the correlations between sulcus diameter and either the white-to-white or angle-to-angle measurements with unsatisfactory results. Even a multivariate predictive model, taking into account white-to-white, angle diameter, age, sphere, cylinder, anterior chamber depth, keratometry, and corneal thickness, can only predict the sulcus diameter within half a millimeter 75% of the time.
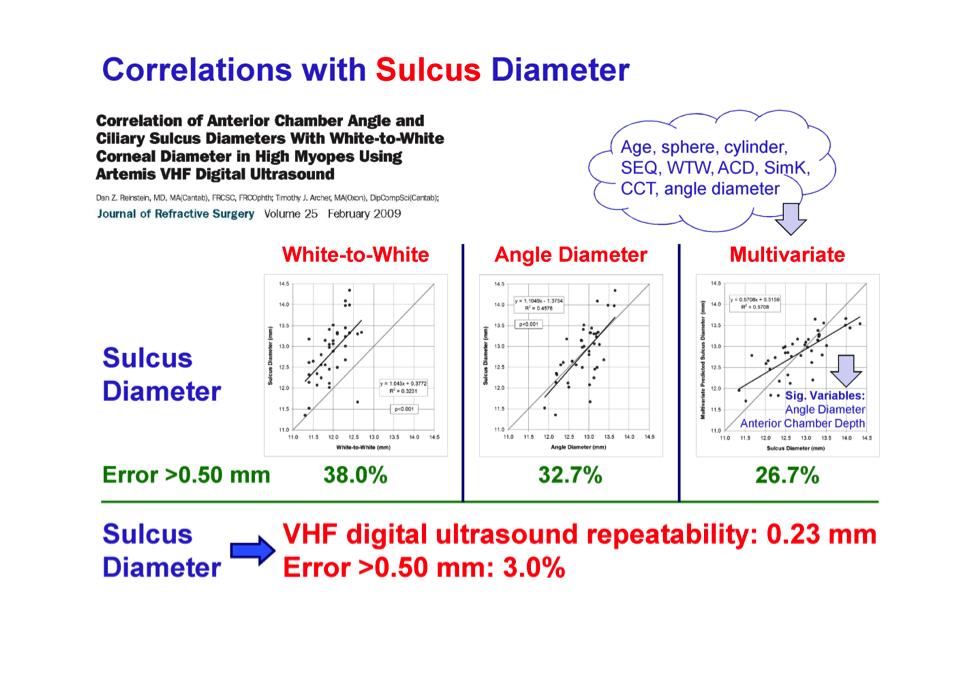
Obtaining measurements via high-frequency ultrasound would require an additional diagnostic device in the office but I think refractive surgeons’ desire for a more accurate measurement tool will drive this technology.
In my view, the Insight100 will benefit the average ophthalmologist who performs LASIK and ICL surgery on the first day this machine is installed. The ability to look behind the iris and physically see ocular structures is also valuable for surgeons who perform complex repair work.
Potential on the Horizon
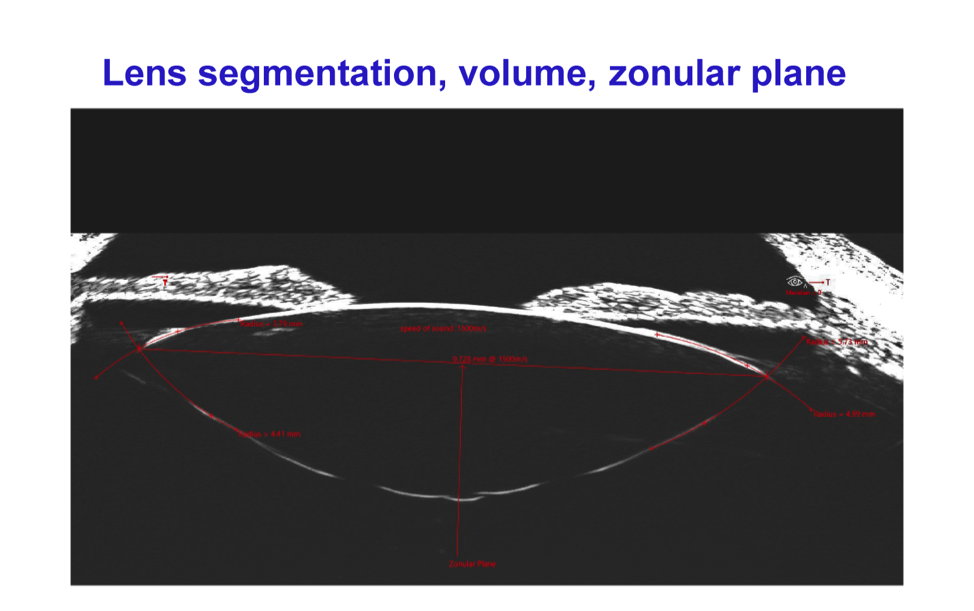
Another developing application for high-frequency ultrasound is in the area of effective lens position (ELP). ELP is the single most important factor that we are not accounting for in IOL power calculations.
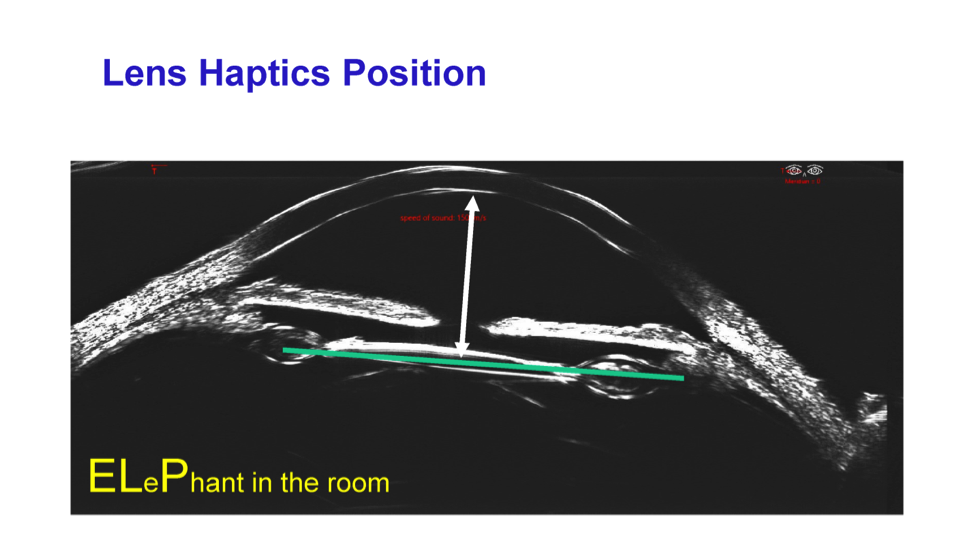
The Insight100 has a “6-degrees of freedom” scanning system, which means it can scan the entire capsule of a crystalline lens and zonular complex to determine the volume of the lens and all of its parametrics.
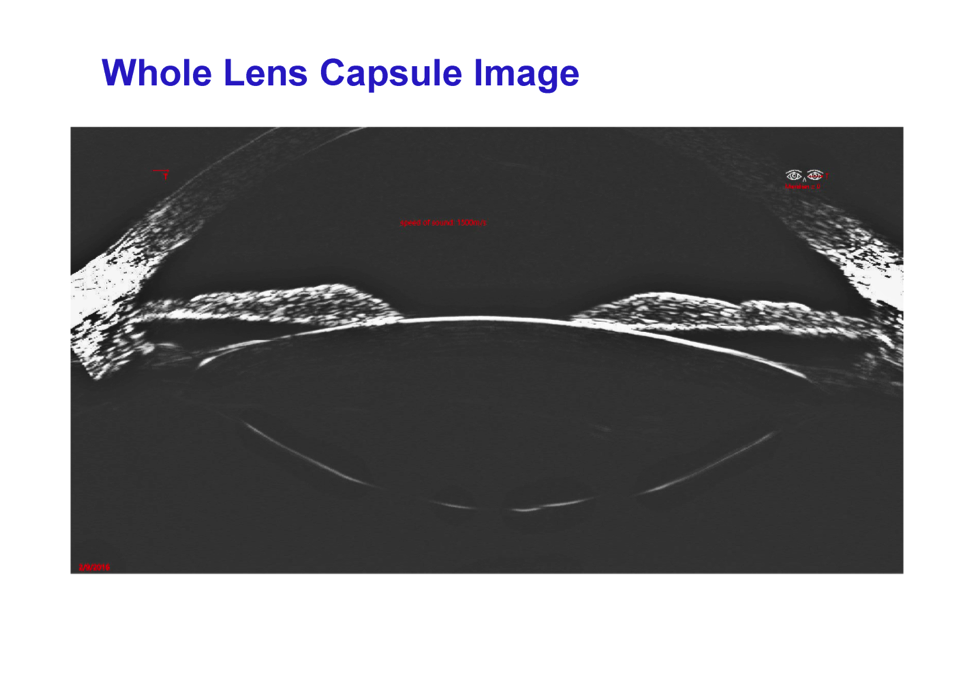
With a high-precision device such as this, the exact orientation of the crystalline lens can be determined preoperatively and it is only a matter of time before researchers ascertain how these measurements effect ELP.
The fact that high-frequency ultrasound is now commercially available means that we are entering a new era for anterior segment eye surgery. Until now, many techniques and protocols have been refined by iteration because a tool capable of accurate measurement was not available. Finally there is a biometric device, accurate to the micron, which can enable any surgeon to do precision surgery based on precision measurements.